ISPGR World Congress Program
ABSTRACT PROCEEDINGS
Please note that any further changes to the proceedings will be made post conference. The most up-to-date information is available on the App.
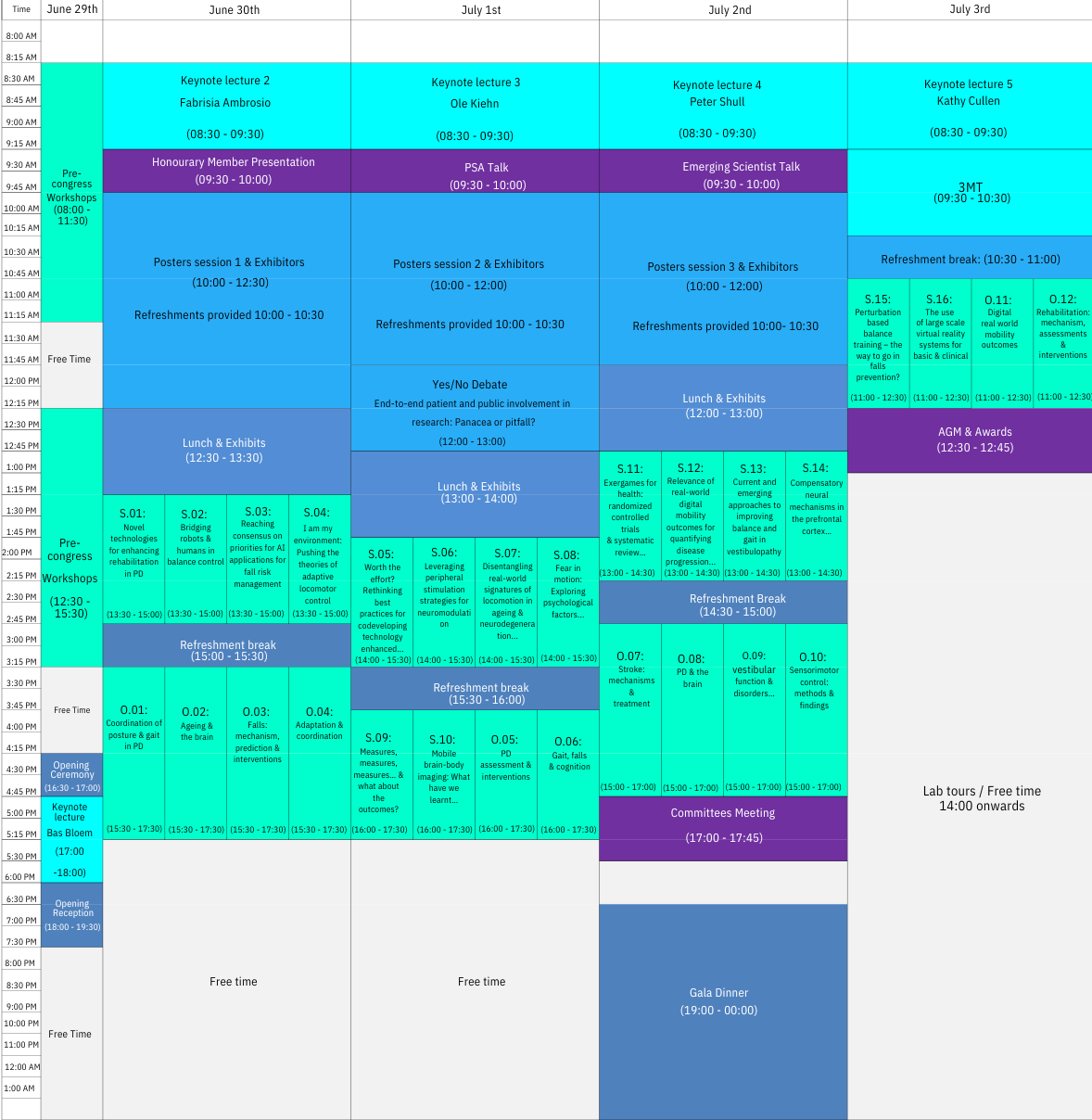
ISPGR Program
ISPGR Detailed Program now available (subject to minor changes)

GUIDED POSTER TOURS OPEN – WALK, TALK, DISCOVER!
WHEN?
Tours start daily at 10:10 AM or as soon as 10 attendees have gathered — First Come, First Served!
WHERE? Meet at the first poster listed on the itinerary.
👉 CLICK BELOW FOR ITINERARIES
LAB TOURS
Attendance at these lab tours is free of charge, but attendees must sign up in advance. Please review the details of each lab tour by clicking in the links below:
PRE-CON WORKSHOPS
SYMPOSIUM SESSIONS
KEYNOTES
POSTERS
Congress Program:
2025 Theme: Productive Interactions
This year the ISPGR will place a special emphasis on building New Connections from Muscles to Minds to Drive Discoveries in Posture & Gait Research.
Special events to foster productive interactions include:
- Guided poster tours
- Local lab tours
- Mentor-mentees activities
Pre-Congress Workshops
8:30AM - 11:30AM: WS.1 - Bridging the gap: best practices in mobile brain imaging
Vivian Weerdesteyn ¹, Bettina Wollesen ², Tjeerd Boonstra ³, Janna Protzak ⁴
¹ Radboud University Medical Center, ² University of Hamburg, ³ Maastricht University, ⁴ Emory University & Georgia Institute of Technology
By participating in this workshop, attendees will learn how to implement mobile brain-body imaging (MoBI) in their studies, broadening the scope of gait research and its applications. This event is designed to bridge current knowledge gaps for those interested in incorporating mobile neuroimaging into their projects, enabling them to explore more diverse research questions and empowering them to contribute to the rapidly growing field of MoBI. MoBI presents unique and complex challenges. While solutions and rationales are starting to emerge in more complex study designs, the field is still developing. This workshop aims to equip participants with the necessary information and expertise to enter the field of MoBI, supporting their learning process.We will start with a concise overview of EEG and fNIRS signals, including what can be measured, how it can be measured, and the advantages and considerations specific to MoBI experiments. Participants will be shown how to set up multimodal recordings with either EEG or fNIRS in combination with IMUs and video tracking and potentially more devices. We will explain the LabStreamingLayer (LSL) protocol for synchronizing devices in real time. Next, participants will have the opportunity to record either EEG or fNIRS in combination with other modalities (e.g. movement) in one of the two parallel tracks. This section will address essential setup skills, including signal optimization and integrating LSL streams on recording devices. In the fNIRS track, participants will have the opportunity to set up and collect fNIRS data on a participant to learn the fundamentals of optode installation and signal optimization and be equipped with the skills to record high-quality fNIRS MoBI data. In the EEG track, participants will be able to record mobile EEG data and do real-time signal quality cleaning using artifact subspace reconstruction. After data collection, we will continue in parallel tracks and focus on data (pre-)processing of pre-recorded fNIRS or EEG data. For fNIRS, we will explain key steps in the current landscape of fNIRS MoBI (pre-)processing such as motion artifact correction and short channel regression, applying them to our pre-recorded data step by step, equipping participants with the theory to apply to their own unique MoBI study designs. With the data cleaned, we will conduct an analysis explaining key concepts of the generalized linear model and quantifying changes in cortical activity with fNIRS. For EEG, we will present the different steps for going from raw mobile EEG data to clean, interpretable data suitable for statistical testing. Emphasis will be on visualizing the effects of different (pre-)processing steps on the data. Furthermore, we will showcase how to identify different types of artifacts (muscle, ocular, motion), their properties, and how to minimize their contribution to the data by relying on independent component analysis. In addition, we will explore techniques for deriving and interpreting gait-related neural activity from the cleaned data and how to take into account within-subject and between-subject variability in gait events when analyzing data in the time-frequency domain.The workshop will conclude with a collaborative discussion on the common pitfalls and challenges encountered in MoBI experiments. Experienced researchers will share their insights and practical tips, thereby fostering a deeper understanding of best practices in the field. Participants will have the opportunity to engage in an interactive session, during which they can ask questions and collectively explore strategies for overcoming the unique challenges posed by mobile brain imaging. This final session will provide a valuable platform for knowledge exchange and networking, to enable attendees to embark on their own MoBI research endeavours with confidence. Proposed Format of the Workshop1. Introduction (5 minutes)Vivian WeerdesteynIntro to mobile brain imaging and its potential.2. Multimodal setups (35 minutes)fNIRS: Sue PetersEEG : Julius Welzel, Vaishali VinodOverview of EEG and fNIRS data synchronization with LSL.3. Data collection (50 minutes)fNRIS : Konstantinos Tsikrikis EEG: Joris van der Cruijsen, Julius Welzel, Vaishali Vinod, Natalie RicherHands-on mobile fNIRS or EEG data collection in combination with other modalities.4. Data (pre-)processing (60 minutes)fNIRS : Konstantinos TsikrikisEEG : Joris van der Cruijsen, Julius WelzelExample data (pre-)processing.5. Wrap-up (30 minutes)fNIRS: Sue Peters, Konstantinos TsikrikisEEG: Natalie Richer, Bettina WollesenPitfalls, practical considerations, and potential study designs. Special requirements for audio-visual needs or materials- Large room for hands-on activities to provide smaller groups with interaction with the equipment.- Screen to project slides and demo analysis onto.- Wifi and outlets
8:30AM - 11:30AM: WS.2 - Central Sensory-Motor Integration balance assessments - background, applications and practical demonstration of a virtual reality
Lorenz Assländer ¹, Chris Easthope Awai ², Robert Peterka 3, Saskia Neumann 2, Jae Lee 4, Laurie King 4
¹ Universität Konstanz, ² Lake Lucerne Institute, 3 VA Portland Health Care System, 4 Oregan Health & Science University
The overall aim is to enable participants to perform Central Sensory-Motor Integration assessments, which provide detailed insights into the sensory integration and feedback control mechanism underlying balance. The goals of the workshop are to 1) provide a basic understanding of the theoretical background of CSMI tests, 2) provide practical examples of how those tests can be used to understand balance disorders and evaluate intervention effects, 3) enable participants to conduct such tests, and 4) to interpret results. The workshop will start with theoretical input, followed by a practical session where we will together run experiments, analyze the data and interpret results. Sessions will be interactive and will allow for ample discussion.
8:30AM - 11:30AM: WS.3 - Cognitive-motor dual-task research: Theoretical foundations, moderating factors, and data interpretation
Ralf Krampe: KU Leuven (Brain & Cognition);
Mihalis Doumas: Queen’s University Belfast (Psychology);
Moran Gilat: KU Leuven (Rehabilitation Sciences);
Karen Li: Concordia University (Psychology);
Moderator: Alice Nieuwboer: KU Leuven (Rehabilitation Sciences);
We aim to provide attendees with insight into the various choices and issues that come with developing technology-assisted, task-specific experimental, assessment and training protocols for walking. We aim to provide attendees with the following main takeaways:Knowledge of the potential factors contributing to protocol designAwareness of the consequences of common choices related to these factorsTips from the speakers not necessarily available in published articlesFeedback and helpful discussion of attendee questions and protocolsPractical demonstrations and examples with many of the protocols and technologies discussed
12:30PM - 3:30PM: WS.4 - Designing technology-assisted, task-specific protocols for walking experiments, assessments and training
Christopher McCrum ¹, Melvyn Roerdink ²
¹ Maastricht University, ² Vrije Universiteit Amsterdam
The need to study, assess and train walking in a task-specific manner is present in many contexts. The skills needed to negotiate the environmental challenges encountered in daily life differ depending on the situation and the person. With advances in technology, the possibilities to create protocols for studying, assessing and training the ability to adapt walking to meet environmental constraints (like avoiding obstacles) and to maintain or recover balance while experiencing disturbances while walking (like tripping) have increased enormously. With this increase in possibility, however, come many decisions and considerations in the process of designing such protocols, whether for the purpose of experiment, assessment or training. These might include the walking speed at which a task should be conducted, the type, difficulty, scaling or pre-knowledge of the task, not to mention how each of these might be increased or varied within and across training sessions and how all of these decisions combine and contribute to effectiveness, feasibility and acceptance of the approach. The full decision-making and piloting process of these decisions, or their theoretical justifications are often not reported in research articles. As a result, for people new to the process of designing such protocols, this can be a daunting task.In this workshop, we aim to provide attendees with insight into these issues. We will start with four presentations from our speakers. Our speakers have each spent considerable time developing and researching devices and protocols related to proactive gait adaptability and reactive gait recovery using different technologies. Each speaker will discuss their own experiences and share their own perspectives, struggles, tips and tricks, in the hope that this is helpful for attendees in their own work. This will be followed with interactive breakout discussions focused on the questions and planned or established protocols of the attendees (a questionnaire will be sent out in advance to gather questions and topics of interest for the interactive discussion). Finally, we will transfer to the gait and balance labs across the road at Maastricht University for some demonstrations and further practical discussions and “feet-on” experiences centred on some of the technologies and protocols discussed by our presenters. Target Audience: Researchers or practitioners (relatively) new to designing and implementing technology-assisted, task-specific experiments, assessments and training of balance and walking. The workshop will be most useful to attendees still in the planning/piloting phase of their projects, but all interested are welcome! To allow for interactive discussion and feedback for each attendee, the workshop will be limited to 32 attendees. Takeaways: Knowledge of the potential factors contributing to protocol design Awareness of the consequences of common choices related to these factorsTips from the speakers not necessarily available in published articles Feedback and helpful discussion of attendee questions and protocols Practical demonstrations and examples with many of the protocols and technologies discussed
12:30PM - 3:30PM: WS.5 - The assessment of proprioception in patient populations, and its relevance for balance
Pieter Meyns ¹
¹ Hasselt University (UHasselt)
1. Understanding of Proprioception
Definition and Mechanisms: Attendees will gain a thorough understanding of proprioception (conscious and unconscious) and its modalities. Proprioception’s Role in Functional Movement: Attendees will understand how proprioception affects both conscious and unconscious control of posture and balance, playing a vital role in the prevention of falls.
2. Identification of Proprioceptive Deficits in Patient Populations Understanding normal proprioceptive functioning across the lifespan: Attendees will also gain insight into proprioception in healthy individuals across different age categories.
Understanding Common Patient Populations: Attendees will be able to identify patient populations that are most likely to experience proprioceptive deficits. Clinical Symptoms of Proprioceptive Dysfunction: Participants will learn to recognize clinical signs and symptoms of proprioceptive dysfunction.
Impact on balance: Attendees will gain insight into how proprioceptive deficits specifically affect posture and balance.
3. Proprioception Assessment Tools and Techniques. Assessment tools and techniques: Attendees will become familiar with a range of tools and assessment methods to evaluate both conscious and unconscious proprioception.
Interpretation of Results: After practicing assessment techniques, attendees will understand how to interpret the results and identify proprioceptive deficits. They will learn the benefits and pitfalls of the different tools and techniques.
Conclusion:By the end of the workshop, participants will have gained practical, evidence-based skills and knowledge in assessing proprioception in healthy and patient populations, understanding its impact on balance. They will be equipped to apply these insights across diverse clinical settings, enhancing patient care and rehabilitation.
12:30PM - 3:30PM: WS.6 - Muscle-brain crosstalk as a driver of mobility resilience
Teresa Liu-Ambrose ¹ Caterina Rosano 2,
¹ University of British Columbia, 2 University of Pittsburgh
Although mobility declines with aging, some individuals maintain mobility better than others, despite age- or disease-related challenges. We characterize these individuals as “mobility resilient”. Similarly, there is variation in response to interventions, such as exercise, aimed at improving mobility outcomes in older adults. Factors contributing to these inter-individual variabilities are not well understood. Effective mobility is the end result of the functional capacity of multiple systems, but the unique modulatory and adaptive capacity of central nervous and musculoskeletal systems may provide clues to answer these questions. There have been exciting new insights about the cross-talk between the central nervous and skeletal muscle systems, such as mitochondrial function, myokines, and extracellular vesicles.
This pre-conference workshop intends to increase the knowledge of brain-muscle cross-talk as it relates to mobility and rehabilitation, and molecular mediators as novel intervention targets. We will first summarize the knowledge in the field of brain-muscle cross-talk. Attendees will learn how the central nervous and muscle systems, individually and in combination, may drive mobility resilience. We will highlight the endocrine properties of the skeletal muscles and their impact on the brain. This will serve as a foundation for our speakers who will present clinical trial of exercise with data on muscle, brain, myokines, and functional outcomes. We will then extend the existing brain-muscle cross-talk to include extracellular vesicles – possible and novel mediators of the brain-muscle cross-talk.
The overarching goal of the proposed activities is to convene experienced scientists, new investigators, and trainees to exchange knowledge and ideas and to advance the area of muscle-brain cross-talk to promote mobility resilience.
Symposium Sessions
June 30
13:30 – 15:00
S.01: Novel technologies for enhancing rehabilitation in Parkinson's disease
Rosie Morris ¹, Moran Gilat ²
¹ Northumbria University, ² KU Leuven
Speakers:
Rosie Morris, Northumbria University; Martina Mancini, Oregon Health & Science University; Terry Ellis, Boston University; Alice Nieuwboer, KU Leuven
Parkinson’s disease (PD) is a common neurological condition affecting one in 350 adults. Although medications are effective at alleviating some symptoms, medications are relatively ineffective for treating balance and gait impairments as well as falls. Rehabilitation, including physiotherapy and different forms of exercise, have shown to be beneficial for improving mobility and falls in people with PD (PwPD). In more recent times, there has been focus on the move to integrate technology into rehabilitation to provide therapy that is more personalized, interactive and motivating. Technology allows for a more streamlined approach and easier personalization as it can provide instant feedback on real-time performance and can help to promote condition self-management. The aim of this symposium is to explore different types of technology, how they can be implemented, and improve rehabilitation for PwPD. Speakers will each explore different technologies. Dr Martina Mancini will discuss a personalized tactile cueing system, co-designed by stakeholders, to improve gait and turning and alleviate freezing of gait (FOG). Dr Terry Ellis will present on soft robotics utilising mechanical assistance to avert FOG, Dr Ellis will also discuss implementation of an autonomous closed-loop music auditory stimulation system. Dr Alice Nieuwboer will discuss the use of technology to promote adherence of daily walking activity through lifestyle interventions and the influence of motor and non-motor disease characteristics on the use of technology, for example touch screen devices. Dr Rosie Morris will discuss the role of technology for disease self-management and as a measurement tool. Dr Morris will present on a co-designed app for falls reporting to be utilised by patients, in clinical practice and the research setting. The symposium will explore the advantages and disadvantages and discuss the barriers and enablers of incorporating technology into rehabilitation for PD both in the context of healthcare systems and self-management tools. The future direction of technology in rehabilitation in Parkinson’s will also be discussed. The symposium will first outline rehabilitation in PwPD, providing a brief overview of current examples of rehabilitation. A polling app will be used gain audience views on the use of technology in rehabilitation and current readiness for implementation. The four speakers will present on examples for novel technologies for rehabilitation. Following the final presentation, the moderator will lead the discussion incorporating speakers and the audience. An interactive poll will take place to determine whether opinions of the audience have changed following the symposium. We believe that technology has an important place in future rehabilitation. This novel symposium will provide an overview of technology for PwPD, but importantly discussions will take place to further understand barriers we need to tackle in our future research as a congress.
S.02: Bridging robots and humans in balance control
Noel Keijsers ¹
¹ Department of Research, Sint Maartenskliniek, 6500 GM Nijmegen, The Netherlands
Speakers:
Noel Keijsers, Department of Research, Sint Maartenskliniek, 6500 GM Nijmegen, The Netherlands; Aaron Young, Georgia Institute of Technology; Edwin Van Asseldonk, University of Twente, Faculty of Engineering Technology, Enschede, the Netherlands; Nuria Pena-Perez, RWTH Aachen
Many people with [AEv(E1] neurological disorders, such as stroke, spinal cord injury, and cerebral palsy, suffer from balance and gait impairments. Over the past decade, lower-extremity robotic devices such as lower-extremity wearable exoskeletons and robotic devices have made significant advancements in design and control, demonstrating great potential to improve balance and gait impairments in this population. Balance control is a fundamental aspect of both human and robotic ambulation, essential for maintaining stability and adequate response to perturbations. In humans, balance is regulated through a combination of sensory input (such as vision, proprioception, and the vestibular system) and coordinated motor responses that adjust posture and prevent falls. In robotics, balance control often mimics biological processes, using sensors to detect postural changes and algorithms to adjust the robot’s movements in real-time. While the mechanisms differ, the core principles of sensory integration, motor adjustment, and dynamic stability remain central to both fields, fostering innovation and cross-disciplinary advancements. This intersection offers opportunities for mutual learning: robotic research can draw inspiration from human balance mechanisms, while advances in robotic balance control can inform rehabilitation strategies and assistive devices for people with balance impairments.This interactive session will present the current state-of-the-art in wearable robotics focusing on balance control and strategies to enhance human-robot interaction. Presentations will cover diverse approaches, offering a comprehensive perspective on improving balance and gait through robotic innovation.
S.03: Reaching Consensus on Priorities for AI Applications for Fall Risk Management
Kimberley Van Schooten ¹, Pierpaolo Palumbo ²
¹ University of New South Wales, ² University of Bologna
Speakers:
Conor Wall, Northumbria University; Paola Di Florio, University of Bologna; Lloyd Chan, the University of New South Wales
Background, aims and relevance: As the global population ages, the number of individuals aged 60 and older is expected to double, reaching 2.1 billion by 2050. This demographic shift presents significant health, social, and economic challenges. One of the most pressing concerns related to ageing is the decline in balance and mobility, which increases the risk of falls—a leading cause of injury, hospitalisation, and even death among older adults. Safe mobility is crucial for maintaining a high quality of life and promoting healthy ageing. The World Health Organization’s Decade of Healthy Ageing underscores the importance of safe mobility as a key component in the life-course approach to ageing, recognising its vital role in improving the health and well-being of older individuals. Justification of novelty: The World Falls Guidelines (WFG) provide a comprehensive framework for fall prevention and management; however, many current strategies are limited by the availability of interventions and accuracy of risk assessments. Artificial intelligence (AI) has the potential to significantly enhance fall risk management by improving the precision, scalability, and personalisation of interventions. AI can transform how we detect fall risk, monitor patients, and design individualised prevention strategies. However, effective integration of AI into fall risk management requires a clear understanding of the priorities, challenges, and areas for development within the field.This symposium aims to bring together experts from various disciplines—AI research, clinical practice, and gerontology—in an interactive format to define and prioritise the future of AI in fall risk management. By identifying key challenges and opportunities, this session will contribute directly to the work of the Topic Group on Falls in Older People of the ITU/WHO/WIPO Global Initiative on AI for Health. The goal is to build consensus on the next steps for AI applications in fall risk management, culminating in a collaborative publication that will serve as a framework for advancing AI in this critical area of healthy ageing. Brief outline of format: The session will feature informative presentations and interactive discussions. Each speaker will give an 8-minute talk on AI’s role in fall risk management, with 2 minutes for audience Q&A. The main component will be interactive priority-setting rounds, facilitated by moderators Pierpaolo Palumbo and Kim van Schooten. Live polling and structured discussions will identify key challenges, opportunities, and research priorities. Polling questions will capture diverse perspectives, with real-time results displayed to encourage dynamic conversation. Audience feedback will shape the session, ensuring collaboration on the pressing needs and future directions for AI in this field. The session will conclude with a 5-minute summary of key outcomes, consensus points, and future collaboration opportunities.
S.04: I am my environment: Pushing the theories of adaptive locomotor control
Anne-Hélène Olivier ¹
¹ University of Rennes 2 – Inria
Speakers:
Bradford Mcfadyen, Université Laval; Jonathan Dingwell, Pennsylvania State University; Michael Cinelli, Wilfrid Laurier University; Anne-Hélène Olivier, University of Rennes 2 – Inria
There is no better example of the person-environment relationship than locomotor adaptation; it requires the ability to adapt our movement to the environment or, alternatively, adapt the environment to our movement in order to move about safely, and with purpose. Research on adaptations specific to locomotor movements has studied different environmental contexts from collision avoidance to interception to path geography requiring anticipatory and reactive visuo-locomotor control. This research has also considered a variety of personal (training, sex, age, cognitive and physical deficits) and environmental (static and dynamic physical constraints, affective issues) factors using protocols designed in real and virtual environments. Yet, this research is still relatively young and based on different theories about the sensori-locomotor control underlying the adaptation of locomotion for the environment. This symposium provides an opportunity to bring together experts to exchange and debate on the visuo-locomotor control underlying our ability to adapt to the environment. While focused around locomotor navigation of our space, the discussion of this symposium has greater interest in general adaptive locomotor control (i.e, stepping over obstacles or up/down stairs). The symposium will provide different points of view on anticipatory and reactive control in relation to theories of affordances, internal models and active inference with the common goal of seeking control variables that are generic or specific to the environments that define us and our movements.
July 1
14:00 – 15:30
S.05: Worth the Effort? Rethinking Best Practices for Co-Developing Technology-Enhanced Training Approaches
Patrick Manser ¹
¹ Karolinska Institutet
Speakers:
Patrick Manser, Karolinska Institutet; Eling De Bruin, OST St.Gallen & IBWS ETH; Jean-Jacques Temprado, Aix Marseille Université; Erika Franzén, Karolinska Institutet
Innovations in digital health technologies, such as motion-based or exergaming technologies, have been recognized as a promising avenue for health promotion and disease prevention across various populations and age groups. Currently, a paradigm shift is occurring in the field, moving from the application of off-the-shelf recreational technologies or (exer)games, primarily designed to make a specific type of activity more fun and entertaining, towards purposefully developed technology-enhanced training concepts. To support this paradigm shift, in this symposium, we will rethink best practices for the co-design, purpose-development, and evaluation of individually tailored technology-enhanced training concepts. We aim to support the credibility and robustness of our field by addressing the topic as follows: First, we will introduce the topic and present a controversial paper, “The dark side of coproduction: do the costs outweigh the benefits for health research?”. Then, we will start a polling app that allows for continuous voting of “pro” versus “contra” co-development throughout the symposium. Second, we will critically reflect on available methodological guidelines aimed at supporting the development and evaluation of complex interventions. We will share our key challenges and learnings from one completed (‘Brain-IT’; Presentation 1 – Prof. Dr. Eling D. de Bruin) and one ongoing project (‘Silver Explorer’; Presentation 2 – Prof. Dr. Jean-Jacques Temprado) implementing these guidelines and elaborate on the relevance for rethinking best practices. Third, we will moderate a first panel discussion on the underlying reasons and viewpoints of “pro” versus “contra” co-development voters (team of five “pro” and five “contra” voters; each consisting of four members from the audience and one symposium author).Fourth, we will present the Co-Develop-IT2 guideline (Presentation 3 – Dr. Patrick Manser). This consensus-based methodological guideline proposes best practices for the iterative Co-design, Purpose-Development, and Evaluation of Individually Tailored Technology-Enhanced Training Concepts. Its unique feature is the inclusion of a checklist to support the effective implementation of the guideline. Fifth, we will present two ongoing projects in the field of hybrid or home-based exergame-based training with a focus on developing a personalized and individually tailored precision rehabilitation concept (Presentation 4 – Prof. Dr. Erika Franzén) and the integration of simultaneous motor-cognitive exercises (Presentation 5 – Lotte Hardeman) for Parkinson’s disease as application examples of the implementation of the Co-Develop-IT2 guideline. Finally, we will analyze and critically reflect on the changes in the proportion of “pro” versus “contra” co-development voters that occurred during the symposium and moderate a second part of the panel discussion focusing on the novelty, practicality, and potential impact of the Co-Develop-IT2 guideline.
S.06: Leveraging peripheral stimulation strategies for neuromodulation of reactive balance responses
Tanvi Bhatt ¹
¹ University of Illinois at Chicago
Speakers:
Brye Mcmorran, Northwestern Polytechnic; Tamaya Van Criekinge,, Maastricht University
Reactive balance control is essential for postural stability, enabling recovery from unexpected perturbations through compensatory stepping or feet-in-place responses. Impairments in this domain significantly increase fall risk and loss of independence in older adults and individuals with neurological disorders. This symposium investigates three neuromodulatory approaches—mechanical vibration, galvanic vestibular stimulation (GVS), and functional electrical stimulation (FES)—that independently target distinct neural and biomechanical mechanisms of reactive balance control. By exploring these modalities, we aim to advance understanding of the neuromechanisms underlying reactive balance and develop tailored interventions to optimize perturbation-based training. The findings have direct relevance for clinical rehabilitation, offering innovative strategies to improve fall resistance and functional outcomes in at-risk populations. The symposium is unique as it will feature 3 women-expert talks at 3 different career stages and from 3 countries, each focusing on one of 3 independent neuromodulation modalities using peripheral stimulation, each addressing novel aspects of reactive balance control. First, mechanical vibration modulates proprioceptive feedback through sub-threshold and supra-threshold pathways. Sub-threshold vibration enhances balance via stochastic resonance, amplifying sensory signals, while supra-threshold vibration disrupts balance and engages compensatory mechanisms. In this symposium discussing the dual role of vibration as a priming tool and perturbative stimulus makes vibration both innovative and contentious in reactive balance rehabilitation. Second, GVS uniquely manipulates vestibular input by altering eighth cranial nerve activity, offering insights into the vestibular system’s contributions to reactive balance strategies. We will highlight studies pairing GVS with whole-body perturbations and its influence on stability, step mechanics, and scaling the response according to the direction of the sensed illusory GVS motion.. Third, synchronously delivering FES during perturbations, represents a novel method for improving stability and limb support while advancing neuroplasticity in individuals with impaired motor control. We will present evidence to support the postulation that by strengthening corticospinal connectivity and facilitating motor adaptation, FES emerges as a transformative tool for enhancing reactive balance. Through this multidisciplinary investigation, the symposium offers a foundation for developing multimodal rehabilitation frameworks. The Moderator will facilitate a dynamic scientific exchange on research implications, future directions, and translating findings into practical applications. Audience interaction will be encouraged through polling, Q&A sessions, and small group breakout discussions to explore implementation challenges and opportunities.
S.07: Disentangling real-world signatures of locomotion in ageing and neurodegeneration: from disease-specific early signs to decreased functional mobility
Lisa Alcock ¹, Winfried Ilg ² ³
¹ Newcastle University, ² Hertie Institute for Clinical Brain Research, Tübingen, Germany, ³ Hertie Institute for Clinical Brain Research
Speakers:
Kimberley Van Schooten, University of New South Wales; Riona Mc Ardle, Newcastle University; Lisa Alcock, Newcastle University; Winfried Ilg, Hertie Institute for Clinical Brain Research, Tübingen, Germany
Maintaining mobility is fundamental to health and physical function, social interactions and independence, and quality of life. Reduced or impaired mobility is common in older age and in the presence of pathology. Gait and turning are two components of mobility that have received significant attention in both lab and real-world research and across a range of patient cohorts, with growing evidence supporting their clinical utility.In this symposium, we will provide an update on current research investigating real-world mobility using wearable sensors in older adults and individuals at risk of falls, as well as a range of neurodegenerative disorders (cerebellar ataxia, dementia, Parkinson’s disease). Outcome selection is critical – linking discrete mobility outcomes to established measures of functional mobility and patient-reported outcomes is an important focus for adoption in clinical trials. Evidence supporting the use of real-world mobility outcomes will be summarized and gaps in our understanding highlighted. Synthesizing evidence across pathologies will allow specific signatures of mobility impairment in everyday life to emerge.Recent findings from real-world mobility monitoring will be highlighted in four 15-minute presentations: 1. Dr Kim van Schooten will talk about identifying faller profiles using real-world ambulation; 2. Dr Ríona Mc Ardle will talk about using real-world gait signatures to aid in the differential diagnosis of dementia subtypes; 3. Dr Lisa Alcock will talk about the value of real-world mobility monitoring in PD; and 4. Dr Winfried Ilg will talk about tracking disease progression in cerebellar ataxia. A summary of cross-pathology signatures of mobility impairment in the real-world will be provided by the moderator, including gaps in our understanding (i.e. responsiveness of outcomes). The final 20-mins of the symposium will be dedicated to interactive, scientific exchange with the audience.As a society, ISPGR comprises researchers with a shared interest in the investigation of gait and posture. Promoting the use of wearables for real-world mobility monitoring is important in the context of ageing and pathology, and applicable to many important clinical questions (ie. supporting diagnosis, identifying individuals at risk, tracking disease progression, response to intervention). This symposium will appeal to a wide audience of ISPGR attendees. Harnessing the collective understanding of mobility monitoring across different patient cohorts and clinical applications enables knowledge to be shared to advance progress in this important research area.
S.08: Fear in motion: Exploring psychological factors behind falling in older adults and neurodegenerative conditions
Taylor Takla ¹
¹ Wayne State University
Speakers:
Taylor Takla, Wayne State University; Nora Fritz, Wayne State University; Jason Longhurst, Saint Louis University; Daniel Peterson, College of Health Solutions, Arizona State University, Phoenix, AZ, USA; Toby Ellmers, Imperial College London
Falls are an unfortunate commonality among older adults and persons with neurodegenerative diseases (NDD). Though the downstream impacts of falls (reduced activity, poorer mental health, declining function) are widely recognized, the role of psychological contributors to falls and subsequent decline remains comparatively understudied. Psychological factors, including fear of falling (FOF), avoidance behaviors, and balance confidence contribute to increased fall risk in older adults and NDD, yet effective interventions remain sparse, making this a crucial discussion topic. Psychological factors often contribute to a vicious cycle of physical inactivity, avoidance, deconditioning, fear, and increased fall risk. However, not all fallers develop fear or avoidance, and some non-fallers do. This session will explore 2 key questions central to understanding and managing psychological contributors to falls: 1. Are falls and FOF always “bad”? We will broaden the concept of a “bad” fall to include not only physical injury, but also emotional insults, such as the embarrassment or distress caused by falling, and the potential for falls to trigger the vicious cycle. Data will be presented to support opposing viewpoints that all falls are bad vs. some falls are not bad. We will debate whether the goal of rehabilitation should aim to reduce all falls, or if efforts should prioritize preventing the “bad” falls that result in injury (physical or emotional) or escalate the vicious cycle. Additionally, we will explore whether a certain level of concern about falling may be beneficial, acting as a protective mechanism that encourages cautious behavior and fall risk reduction strategies. 2. When considering psychological contributors to falls, what matters more – perception or physiological ability? Not all fallers develop fear and avoidance behaviors, and some non-fallers experience it. Data will be presented to support opposing viewpoints that perception matters more vs. physiological ability matters more. We will discuss how a mismatch between perceived and actual fall risk may help explain who is most likely to enter the vicious cycle, as well as downstream consequences of this mismatch. Furthermore, we will discuss whether a fall could serve as a “reality check”, leading to a beneficial realignment of perception and behavior. We will consider whether rehabilitation should target perception, physiological function, or both to reduce fall risk. Finally, we will discuss models of FOF in light of the recent discussion, followed by a discussion of a new harmonized model that incorporates missing components highlighted in the presentation. Through interactive debate, we aim to identify novel perspectives and recommendations for future research and clinical practice to guide more effective assessments and interventions for reducing falls and negative psychological consequences in both older adults and NDD populations.
July 1
16:00 – 17:30
S.09: Measures, measures, measures… and what about the outcomes?
Claudia Mazzà ¹
¹ Indivi
Speakers:
Charalampos Sotirakis, Nuffield Department of Clinical Neurosciences, University of Oxford (UK); Luca Palmerini, University of Bologna; Matthew Jones, University of Sheffield; Silvia Del Din, Newcastle University
Digital technologies nowadays dominate mobility and behavioral research: collecting data has become easy and so is the generation of very large datasets, often containing redundant and not always robust information. Signal processing, Machine Learning and AI techniques in general are simultaneously evolving to support interpretability and readability of this data. Nonetheless, the problem of translating these measures into meaningful outcomes that are ready for use as endpoints in drug trials or for clinical diagnosis and treatment as part of routine clinical practice remains an open challenge. This is associated to both complex validation processes, including both technical and clinical aspects, but also to the need of establishing and retaining measure meaningfulness in each context of use. In this symposium we will explore possible approaches to transform measures into explainable outcomes, with the goal of eliciting discussion both from an analytical and a clinical point of view. We will do so by presenting applications from different disease areas and data collected with a variety of digital health technologies and experimental protocols. We will present different approaches to extract meaningful information from the high-dimensional data in different contexts and reflect on how even the definition and measure of gait might have to be adapted according to the specific question at hand. We will also present an example of how the success of these efforts in the gait analysis field might lie in the ability to import advanced analyses techniques from other, non-obviously adjacent, fields. Finally, we will hold a discussion on theoretical and practical approaches to building trustworthy and transparent outcomes that can shape the clinical decision-making. The overall goal is to trigger a discussion on different approaches to select the most relevant information from the redundant array of measured gait characteristics.
S.10: Mobile brain-body imaging: What have we learnt about the neural control of human balance and gait?
Tjeerd Boonstra ¹, Klaus Gramann ²
¹ Maastricht University, ² Berlin Institute of Technology
Speakers:
Daniel Ferris, University of Florida; Dante Mantini, Katholieke Universiteit Leuven; Huiling Tan, University of Oxford; Vivian Weerdesteyn, Radboud University Medical Center
Traditionally, gait was viewed as a largely automated function regulated by spinal and subcortical neural circuits. However, growing evidence now highlights the significant role of cortical involvement in walking. Limitations of traditional brain imaging methods long impeded direct investigation of cortical contributions to gait. Mobile EEG has revolutionized this field, enabling the recording of brain activity during actual locomotion. Specifically, Mobile Brain-Body Imaging (MoBI), which integrates mobile brain imaging, EMG, and 3D kinematics, has emerged as a powerful approach to explore the neural mechanisms underlying human gait. Recent studies leveraging MoBI technology have expanded our understanding of cortical control over gait, including its roles in balance, motor planning, and coordination. This growing interest has highlighted the need to discuss the clinical and research implications of these advancements. This symposium will bring together a diverse panel of engineering, neuroscience, and rehabilitation experts, including speakers new to ISPGR, to provide a fresh perspective on gait research. Key topics will include: The technological and methodological advancements in MoBIApplication of brain network analyses to uncover cortical gait control mechanisms. Correlation of findings with local field potentials obtained through invasive recording. Relevance of computational and decision-making processes for rehabilitation Through interactive discussion, we will evaluate the physiological interpretation of metrics derived from mobile EEG during walking and explore how these metrics can be applied in clinical settings to identify mechanisms behind movement disorders.
July 2
13:00 – 14:30
S.11: Exergames for health: randomized controlled trials and systematic review evidence for the effects on physical and cognitive functioning, brain modulation, and informing the designing for healthy and clinical populations
Eleftheria Giannouli ¹
¹ ETH Zurich
Speakers:
Daina Sturnieks, University of New South Wales, Neuroscience Research Australia; Marie-Laure Welter, CHU Rouen, Brain Institute; Eleftheria Giannouli, ETH Zurich; Anna Lisa Martin-Niedecken, Zurich University of the Arts
Exergames—interactive video games that are played with whole-body movements—are emerging as powerful tools to address cognitive and motor impairments in diverse populations, particularly older adults and individuals with neurodegenerative conditions. With the ability to simultaneously target physical and cognitive functioning, exergames offer scalable interventions that can overcome traditional barriers to care, such as access to rehabilitation facilities. This symposium brings together cutting-edge research exploring the efficacy, feasibility, and neurophysiological effects of exergame-based interventions for health. The symposium aims to (1) present robust evidence from randomized controlled trials (RCTs), (2) discuss the mechanisms underlying the observed health benefits, including brain modulation, and (3) offer insights into the design of effective exergame interventions across populations. While exergames have gained attention in recent years, the application of RCTs to rigorously evaluate their effectiveness across multiple domains—physical health, cognitive functioning, and neuroplasticity—is relatively novel. This symposium presents findings from three RCTs and a systematic review, each targeting unique populations and outcomes: fall prevention in community-dwelling older adults, cognitive-motor functioning in older adults with prescription for rehabilitation, and brain modulation in individuals with advanced Parkinson’s disease. Additionally, this session will provide practical insights into the design process of exergames, ensuring they are tailored to meet the needs of specific populations. The interdisciplinary scope of the symposium bridges public health, rehabilitation, neuroscience, as well as game design and game research, making it particularly relevant for researchers, clinicians, and policymakers. The symposium will consist of four presentations, followed by an interactive, moderated discussion with the audience. The first three presentations will focus on the evidence from RCTs and a systematic review. The final presentation will delve into the approaches of designing exergames for health, emphasizing interdisciplinary and user-centered processes. To facilitate scientific exchange, the discussion segment will involve live polling to gather audience perspectives on the key challenges and opportunities for exergames in health promotion and rehabilitation. Additionally, the symposium will include live demonstrations of the exergames, providing attendees with the opportunity to try them out first-hand. This interactive format will ensure a dynamic dialogue, foster collaboration across disciplines, and offer a practical understanding of exergames’ potential for health and rehabilitation. By addressing both evidence and implementation, this symposium aims to advance the science of exergames and highlight their potential as innovative, accessible tools for improving health.
S.12: Relevance of real-world digital mobility outcomes for quantifying disease progression and therapeutic response in Parkinson’s disease and atypical parkinsonian syndromes
Lisa Alcock ¹, Heiko Gaßner ²
¹ Newcastle University, ² University Hospital Erlangen
Speakers:
Alison Yarnall, Newcastle University; Lisa Alcock, Newcastle University; Christian Schlenstedt, Medical School Hamburg; Heiko Gaßner, University Hospital Erlangen
Background: Digital mobility outcomes (DMOs) derived from wearable sensors in standardised settings are highly relevant to complement the clinical assessment of motor symptoms performed by clinicians and patient-reported outcome measures (PROMs). They can objectively capture gait patterns of individuals with Parkinson’s disease (PD) and atypical Parkinsonian disorders (APD). DMOs have been shown to detect disease severity cross-sectionally, but there is a lack of evidence supporting the selection of outcomes for monitoring disease progression and evaluating therapeutic response. Aims, novelty, and relevance: In this symposium, we present the relevance of DMOs in detecting disease progression and treatment effects based on data from the largest real-life data sets available to date. We further discuss challenges and future perspectives of integrating digital technologies in healthcare. Prof. Yarnall will present results as part of the Mobilise-D project (https://www.mobilise-d.eu/), in which we are validating and supporting the widespread adoption of real-world DMOs to monitor mobility-disability, a potential marker of disease progression. It is of utmost importance to enhance our understanding of the dynamic nature of fall risk and falls in a personalised approach using real-world data. This deeper understanding supports us to define targeted interventions to prevent fall risk and falls in PD. Dr. Alcock will present insights gained from discrete measures of gait to identify and mitigate fall risk. Freezing of Gait (FOG) in PD is related to disease progression and associated with loss of mobility and falls. Prof. Schlenstedt will compare cross-sectional and longitudinally collected real-world DMO data between freezers and non-freezers. Furthermore, variations of mobility over the day will be related to FOG, and conversion to FOG will be discussed. Exercise is considered a highly relevant and effective treatment option in PD to ensure stable walking and prevent falls. Therefore, intensive gait-focused exercise is within the focus of the talk of Dr. Gassner (Mobility_APP project). He will evaluate the effects of therapeutic response using gait tests in the hospital and real-life DMOs in a large cohort of APD and PD patients. Format: The symposium will begin with a brief introduction to the importance of real-life mobility monitoring and the relevance of this topic. We introduce the presenters and the topics of each talk. The moderators will present the two stimulating questions using the electronic polling app to engage the audience in critical thinking. Each presentation will last 15 minutes. After the last presentation, the moderators will lead a discussion (20 mins), including all speakers and allowing for questions from the audience. The audience will be encouraged to complete the electronic poll to gain feedback about the lessons learned from the audience. The moderators will conclude the session.
S.13: Current and emerging approaches to improving balance and gait in vestibulopathy
Christopher Mccrum ¹
¹ Maastricht University
Speakers:
Anissa Boutabla, Geneva University Hospitals and University of Geneva, Geneva, Switzerland; Klaus Jahn, Schoen Clinic Bad Aibling; Max Wuehr, Ludwig-Maximilians-University Munich; Meichan Zhu, Maastricht University
The vestibular system plays a central role in balance and gait control. Deficits in vestibular function are not confined to isolated cases of peripheral vestibulopathy but are increasingly recognized as a natural consequence of aging and associated with prevalent neurodegenerative disorders, such as Parkinson’s disease. Chronic vestibular hypofunction is now acknowledged as a major cause of balance impairments and fall-related injuries. Recent advancements, including the establishment of diagnostic criteria and technological innovations, have opened new avenues for understanding vestibular pathologies and developing therapeutic approaches that extend beyond peripheral vestibulopathy, potentially serving a broad population of patients with chronic balance impairments. In this symposium, we will discuss the balance and gait-related challenges faced by people with vestibulopathy and discuss the current state of the intervention landscape for improving balance and gait, focusing on physical therapy approaches, as well as on new and emerging technology-assisted approaches such as enhancing residual vestibular function (via noisy galvanic vestibular stimulation) or artificially replacing vestibular function (via vestibulocochlear implants). A common theme throughout the talks will be the need for understanding the specific needs of each patient and tailoring the intervention approaches and content to these needs. Our aim is to both shed light on the specific deficits, needs and options for people with vestibulopathy and to provide the audience with better general understanding of the vestibular system and its role in balance and gait.Following a brief introduction by the Chair, our four speakers will present for about 15 minutes. After each talk, there will be time for one or two specific questions. After the final talk, the remaining 25 minutes will be open for audience questions and discussion, which will be moderated by the Chair. The polling tool will be used to present the audience with a range of topics and questions and based on how many vote for each item, the discussion will focus on the popular items.
S.14: Compensatory neural mechanisms in the prefrontal cortex: attentional resources for gait and balance in aging and mild cognitive impairment
Gelsy Torres-Oviedo ¹
¹ University of Pittsburgh
Speakers:
Gelsy Torres-Oviedo, University of Pittsburgh; Trisha Kesar, Emory University; Tanvi Bhatt, University of Illinois at Chicago; W. Pieter Medendorp, Radboud University Nijmegen
Maintaining balance and mobility is critical for independence in older adults, yet these functions often decline due to aging and cognitive impairment. This symposium examines how attentional control influences locomotion and balance, focusing on the neural and cognitive mechanisms involved. Presentations by four experts will explore the interplay between cognitive and motor systems in healthy older adults and those with mild cognitive impairment (MCI), offering insights into how these systems adapt, or not, to challenging walking situations. Kristan Leech will present foundational theory on motor control and learning, emphasizing mechanisms underlying sensorimotor adaptation for walking automaticity and adaptability. Her research highlights explicit control, forward model calibration, and stimulus-response mapping during locomotor adaptation, crucial for navigating complex environments. Gelsy Torres-Oviedo will discuss attentional control’s role in locomotor adaptability and memory, focusing on dual-task walking and locomotor savings—the ability to retain and reuse prior improvements. While healthy older adults compensate with attentional resources, those with MCI show reduced savings and greater cognitive demands. Neuroimaging links these deficits to basal ganglia dysfunction, shedding light on underlying neural mechanisms. Trisha Kesar expands on the cognition-motor relationship in aging, examining split-belt locomotion, overground gait modulation, and corticospinal neurophysiology. Her findings reveal that cognitive impairment reduces gait adaptability to perturbations and disrupts motor-cognitive integration. Corticospinal excitability studies highlight how cognitive decline reallocates cortical resources for gait and balance. Tanvi Bhatt focuses on reactive balance control and its attentional demands. Her work shows that MCI heightens cognitive demands for reactive balance, particularly during visuomotor tasks. Reduced cerebellar-sensorimotor connectivity and increased cortical network reliance disrupt compensatory mechanisms. Stronger attentional resources improve reactive balance through repeated exposures, paralleling locomotor savings. This symposium synthesizes these perspectives, exploring attentional control as a link between locomotor adaptability, reactive balance, and motor-cognitive interactions. A moderated discussion with live polling and Q&A will address how aging-related deficits alter locomotor and reactive balance savings, strategies for early mobility impairment detection, and interventions targeting attentional control to enhance gait and balance. Panelists will discuss clinical applications, such as dual-task assessments and motor-cognitive training, to improve mobility and reduce fall risk. By integrating research on locomotion and balance, this symposium offers a cohesive framework for addressing mobility challenges in aging and actionable strategies to promote independence in older adults.
July 3
11:00 – 12:30
S.15: Perturbation-based balance training – the way to go in falls prevention?
Jessica Koschate-Storm ¹, Avril Mansfield ²
¹ University of Oldenburg, ² University Health Network, University of Toronto
Speakers:
Michel Hackbarth, University of Oldenburg, Geriatric Medicine; Itshak Melzer, Ben-Gurion University; Hadas Nachmani, Hadassah Medical Center; Yoshiro Okubo, Neuroscience Research Australia
In older adults, falls may lead to severe injuries, limitations in mobility, dependency in daily life, and decreased quality of life. Two meta-analyses suggest that perturbation-based balance training (PBT) appears to be more effective in mitigating the risk of falls among older adults; PBT was reported to reduce fall rate by 40–46% (Mansfield et al. 2015, Devasahayam et al. 2022). PBT is characterized by the use of balance perturbations with sufficient magnitude to induce a fall, if the patient would fail to react with a sufficient sudden motor response (Mc Crum et al. 2022). In this symposium, the current state of PBT-research regarding the effectiveness to reduce fall risk and daily life falls, as well as its feasibility as training intervention in frail older adults and patients will be discussed. A few randomized controlled trials were published concerning the effects of treadmill PBT on daily life falls (e.g. Lurie et al. 2020, Rieger et al. 2024, Norgaard et al. 2023). However, little is known about the task specificity of PBT as well as efficacy and retention in different patient groups (McCrum et al. 2022). Especially the inclusion of participants with cognitive impairment is under debate (Jagropp et al., 2022, Trampisch et al. 2023), and in most studies, older adults with cognitive impairment are excluded from participation. Therefore, an overview of the current literature on the characteristics of PBT to reduce fall risk and falls and increase reactive balance will be presented. Furthermore, characteristics of different perturbation paradigms, recently used in randomized controlled trials will be discussed by the speakers. Afterwards, the study protocol of an ongoing clinical trial, including geriatric patients with and without cognitive impairment, will be described. Since research on effective and scalable fall prevention programs is urgently needed, the symposium will offer the opportunity for valuable discussions on the applicability of different PBT paradigms in fall-prone older adults as well as other target groups in the context of the considerations: is there one optimal PBT intervention for all, and can PBT be introduced to clinical guidelines for fall prevention? Therefore, the availability of sufficient scientific evidence to prescribe perturbation training to prevent falls in daily life will be discussed: which patient groups will benefit most from PBT and how should the training program be designed for different patient groups, especially considering patients with cognitive impairment. Furthermore, it will be discussed what kind of research in the future, to develop a clinical guideline for PBT. First overview of audience’s opinion will be obtained via the polling app, afterwards these topics will be discussed in more detail.
S.16: The use of large-scale virtual reality systems for basic and clinical research of gait and posture
Meir Plotnik ¹, Menno Veldman ²
¹ Sheba Medical Center, ² University Medical Center, University of Groningen
Speakers:
Adi Lustig, Tel Aviv University; Chunchun Wu, University Medical Center Groningen, University of Groningen; Emilia Biffi, Scientific Institute IRCCS E. Medea, Bosisio Parini (LC), Italy; Will Young, Department of Public Health and Sport Sciences, University of Exeter, Exeter, UK
In the background of this symposium are two emerging venues of research. The first is thematic dealing with human behavior as an expression of multi-competency integration, i.e., motor, sensory, cognitive and affect. The second is pseudo- methodological, namely the use of virtual reality (VR) technology for studying perception and action. These two venues are inter-connected, as VR technology allows controlled presentation of stimuli, task contexts, and accurate recording of behavioral response. Our symposium will emphasize the added value of LSVR systems over the common head mount display- based VR technology, in particular in the context of studying and/or rehabilitating gait and posture and their interactions with other motor and non-motor competencies. In LSVR system persons can walk in self-paced mode (more naturalistic), or in fixed speed mode, Force plates, and motion capture systems gather data on locomotion and postural control and on other motor functions, such as gross manual movements, while eye tracking systems complement information on oculomotor function. Cognition can be assessed by exposure to VR context that requires specific cognitive function(s). Adaptations of validated traditional neuropsychological evaluations to VR media create focus for cognitive activity. Affect can be measured with physiological sensors (e.g., electrocardiography, galvanic skin response) reflecting also affect-related effects. Clearly, as will be presented in one of the symposium’s talks (A.L.), the aforementioned features underscore advantages of LSVR systems in studying basic aspects of perception and action. We will present a paradigm centered on innovative validated adaptation of the traditional pen and paper color trails test to LSVR system (VR-CTT). The CTT taps on various cognitive functions. The effect of activation of each domain on gait will be described. In another talk (C.W.) we will show how LSVR can be used to investigate sensory-motor integration. We will present recent data characterizing posture and gait responses to the congruent and incongruent presentations of visual stimuli. We will highlight the applicability of such paradigm to study the effect of physical activity levels in daily life on the ability to modulate gait in response to visual perturbations. Diving even more into the clinical arena (E.B.) we will share the experience with LSVR platforms used to assess gait and balance in pediatric patients undergoing rehabilitation with innovative exoskeletons devices. Finally, presenting highly sophisticated paradigm (W.Y), we will present a study on freezing of gait, an extremely debilitating symptom seen in the majority of persons with advanced Parkinson’s disease, during adaptive gait tasks. This talk will also highlight the pros and cons of using semi-prescribed tasks in VR. To summarize, this symposium underlines the heterogeneity of research and clinical opportunities that LSVR systems behold.