Every neurologist who treats people with Parkinson’s disease knows that his patient has difficulty walking and is at risk for falls. Also, they know that the pharmacological treatment that they will prescribe, levodopa, can only partly improve these symptoms. The neurologist will assess their patient on their ability to walk, their postural instability and will also ask whether they have had any recent falls. In addition to these subjective assessments, more objective measures of gait and balance in PD have been collected in the lab. This wealth of data inspired my colleagues and I to review these more objective studies. Our aim was to evaluate the effect of drugs prescribed to alleviate gait impairment and fall risk in PD.
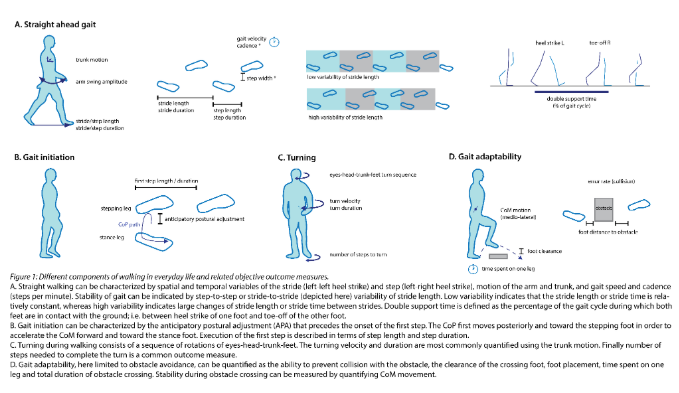
We started this project taking on two positions: First, walking ability in daily life goes beyond gait patterns during straight ahead walking, and should include starting to walk, turning, and avoiding obstacles. Second, people with PD often take medication for other reasons than for PD, as comorbidities are common. Thus, we also wondered what beneficial or detrimental effects these drugs can have on gait in people with PD.
The literature reports quite consistently that levodopa and other dopaminergic medication improve spatial parameters of gait, but not temporal parameters. Other drugs used in PD treatment aim to modulate activity of acetylcholine, glutamate and norepinephrine. Of these drugs, cholinergic agents are the most promising to improve postural instability. Glutamate and norepinephrine drugs are much less studied and show inconsistent findings.
The effect of drugs with sedative or anticholinergic properties – frequently prescribed for bladder problems, pain, or mental health problems – have been widely studied in populations other than PD. These drugs can worsen gait and put people at risk for falls. It is not unreasonable to suspect that these effects would also occur in patients with PD, but this hypothesis remains to be tested.
Unfortunately, there are very few studies that evaluate gait initiation, turning and obstacle avoidance or any walking that is not just straight walking. This is remarkable considering that people with PD are particularly limited in more complex gait tasks than straight ahead walking. Therefore, our review was not able to draw any conclusions on walking ability during more realistic scenarios.
We found serious gaps in the literature. First, walking ability other than straight ahead walking is highly understudied. Secondly, trial designs are largely suboptimal. Studies are either placebo-controlled RCT’s using subjective gait scores, or use objective gait measures but are poorly controlled. It seems feasible to use the best of both ‘worlds’ to improve trial design and further enhance our insights into pharmacological effects on gait and fall risk in PD.
Katrijn Smulders, Marian L. Dale, Patricia Carlson-Kuhta, John G. Nutt, Fay B. Horak. Pharmacological treatment in Parkinson’s disease: effects on gait. Parkinsonism Rel Disorders 2016 vol 31:3-13. https://www-ncbi-nlm-nih-gov.liboff.ohsu.edu/pmc/articles/PMC3923955/
About the Author

Katrijn Smulders
Research department of the Sint Maartenkliniek, Nijmegen
Katrijn’s research in PD has focused predominantly on higher-order control of gait and balance. She completed her PhD at the Parkinson Center at the Radboudumc in Nijmegen (Netherlands) with Bas Bloem and was a post-doc in Fay Horak’s Balance Disorders Lab at OHSU (Portland, OR). At the Sint Maartenskliniek, she studies gait and balance control in orthopedic patients, with a specific interest in the evaluation of orthopedic surgery using objective performance measures.
Copyright
© 2018 by the author. Except as otherwise noted, the ISPGR blog, including its text and figures, is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License. To view a copy of this license, visit https://creativecommons.org/licenses/by-sa/4.0/legalcode.
ISPGR blog (ISSN 2561-4703)
Are you interested in writing a blog post for the ISPGR website? If so, please email the ISGPR Secretariat with the following information:
- First and Last Name
- Institution/Affiliation
- Paper you will be referencing
