Many neurological disorders lead to gait and balance impairments. Especially in older people, these disorders are a common cause of falls, associated with significant morbidity and mortality. Despite the recognition of the socio-economic burden of falls, there are very few treatment options beyond physical therapy for neurological gait and balance impairment. From a brain perspective, human locomotion relies upon a distributed neural network including primary motor, premotor areas, basal ganglia and, importantly, white matter connections between these areas. White Matter hyperintensities and other changes in the cerebral white matter (‘leukoaraiosis’) are very common in old age and associated with gait and balance dysfunction.
This review paper explores whether beneficial effects of physical training can be enhanced by using non-invasive brain stimulation, namely transcranial direct current stimulation (tDCS), in patients with neurological gait disorders. tDCS is a non-invasive neurostimulation technique that consists of delivering a weak electrical current through the scalp. This has been shown to induce bidirectional polarity-dependent changes in excitability of the underlying cortex; anodal tDCS increases cortical excitability and cathodal tDCS decreases it. The physiological and behavioural effects of tDCS have been shown to last for up to one hour, implying that tDCS also modulates the synaptic strength of intracortical and corticospinal neurons.
Across a number of our own pilot studies, we explored whether these physiological and behavioural effects may facilitate neuroplasticity during physical therapy and thus enhance its effectiveness. We applied 15 minutes of anodal tDCS over the motor and premotor cortex of both cerebral hemispheres using a central electrode in patients with Parkinson’s disease and patients with leukoaraiosis while they were also receiving gait and balance physical therapy. We found that the combination of cortical stimulation and physical therapy improved gait velocity, stride length, time taken to complete the ‘Timed Up and Go’, and postural reactions, above and beyond the positive effects of physical therapy alone. tDCS alone (without physical therapy), however, did not improve gait in patients with Parkinson’s disease or leukoaraiosis.
Our review paper and pilot studies suggest that non-invasive brain stimulation (such as tDCS) may enhance the effects of physical therapy in patients with neurological gait disorders. Large-scale, multicenter, randomized, double-blind, Phase III studies using standardized protocols based on the more robust published pilot data are needed before these techniques can be implemented into mainstream clinical practice.
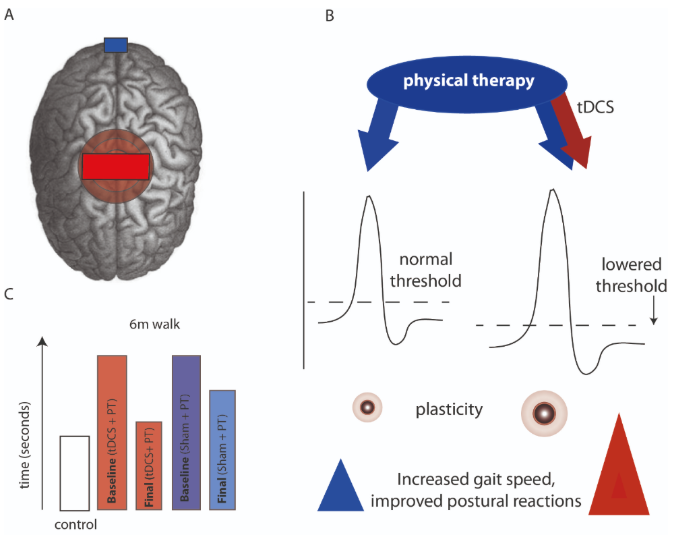
Figure 1. A tDCS stimulation protocol showing anodal tDCS stimulation over the primary motor and pre-motor cortices bilaterally, and reference (cathode) electrode (blue rectangle), over the inion. B Hypothesized effect on synaptic excitability depicting the additive effect of physical therapy and tDCS (red arrow) in lowering the threshold of a motor action potential (i.e. increased cortical excitability), leading to increased cortical plasticity over motor cortical regions, and improved clinical outcomes. C Mean averaged data across pilot studies discussed in the main text, showing the largest reduction in time taken to walk 6 metres in the tDCS + physical therapy arm, compared to physical therapy with sham stimulation.
Publication
Kaski D, Bronstein AM, 2014, Treatments for Neurological Gait and Balance Disturbance: The Use of Non-invasive Electrical Brain Stimulation, Advances in Neuroscience, Vol: 2014, Pages: 1-13, ISSN: 2356-6787
About the Author
Dr Diego Kaski
Consultant Neurologist and Honorary Senior Lecturer, Gait and Balance Lab, Institute of Neurology, University College London
Dr Diego Kaski is a Consultant Neurologist with an interest in Neuro-otology. He completed his PhD investigating the cortical mechanisms underpinning human self-motion perception, and the neural control of gait. His current interests include central vestibular processing and the development of novel treatment strategies to improve gait and balance.
Copyright
© 2018 by the author. Except as otherwise noted, the ISPGR blog, including its text and figures, is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License. To view a copy of this license, visit https://creativecommons.org/licenses/by-sa/4.0/legalcode.
ISPGR blog (ISSN 2561-4703)
Are you interested in writing a blog post for the ISPGR website? If so, please email the ISGPR Secretariat with the following information:
- First and Last Name
- Institution/Affiliation
- Paper you will be referencing
